Islet Transplantation
In islet transplantation, islets are taken from a donor pancreas and transferred into another person. Once implanted, the beta cells in these islets begin to make and release insulin. Other cells help the body maintain acceptable regulation of blood sugar levels that are lacking in other standard therapies such as insulin injections or pumps.
To learn more about the islet isolation process click here or on the menu to the left.
Since islets are kept in culture a couple of days, this allows for selection and admittance of a suitable patient.
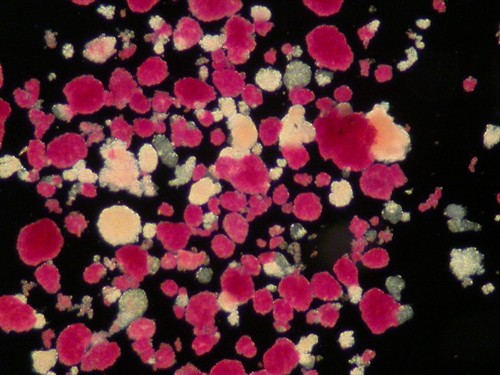 Red-stained,
isolated, human islets of Langerhans. Photo: Andrew
Friberg
Red-stained,
isolated, human islets of Langerhans. Photo: Andrew
Friberg
During the transplant, the radiologist uses ultrasound to guide placement of a catheter through the skin and liver tissue and into the portal vein, the main blood supply of the liver. The islets are then injected through the catheter into the liver. The patient will receive a local anesthetic or general anesthesia. If anatomical or other problems occur, the transplant can be done through a small abdominal incision.
It takes time for the cells to attach to new blood vessels and begin releasing insulin. It is vital that the islets are able to "rest" during this period and insulin will be needed at least until engraftment in the liver is completed (> three weeks).
Benefits and risks
The chance to obtain better metabolic control is the main benefit of islet transplantation. Today, repeated islet infusions are needed to achieve insulin independence. In the Nordic Network we have given up to four transplants and achieved an insulin independence of about 50%. All transplanted patients have become C-peptide positive with a stabilization of their metabolic control and a reduction of their need of insulin therapy. These patients have previously undergone kidney transplantation.
To avoid rejection of the transplanted islets, immunosuppresion is needed. In contrast to other transplantations, steroids and lymphocyte depleting antibodies are avoided in the protocol. Emphasis is put on mycophenolate mophetil (Cellcept®) or sirolimus (Rapamune®) combined with a low-dose calcineurine inhibitor (tacrolimus (Prograf®) or cycloporineA (Sandimmun Neoral®)) and a interleukin 2 receptor blocking antibody (daclizumab (Zenapax®)) used only in the peritransplant period.
Side effects of immunosuppressive treatment includes nephrotoxicity, infections and an increased risk of developing cancer. Patients are closely monitored to avoid these risks and to detect any unfavourable signs early.
The islet transplant itsef is a minor procedure, although partial portal thrombosis and bleedings have been reported. Earlier when larger volumes with more exocrine tissue were transplanted a few cases with total portal thrombosis (blood-clotting) occured.